Rapid Antigen Test
Last updated: January 12th, 2025
What makes a "Rapid Antigen Test" rapid? The best way to explain this is by comparing it to the PCR test.
Rapid Antigen test vs PCR test
PCR (Polymerase chain reaction) tests screen for the presence of viral RNA. This is detectable in the body before antibodies form or symptoms of the disease are present. This means PCR tests can tell whether someone has the virus very early on in their illness. Or not.
Due to its accuracy, the PCR test is the main diagnostic test for COVID-19. This is what the Maltese Health Authorities refer to as "swab tests" in their metrics:

The main downside is that PCR testing relies on expensive and specialised equipment. Collected swabs need to be sent away to a lab for analysis. It can take days for people to find out their results!
How is the Rapid Antigen test done?
Rapid Antigen tests do not need to be sent away for confirmation. The whole procedure can be done in a clinic, doctor’s office, or hospital. In fact antigen tests results are usually known in as little as 15 minutes!
Like the PCR test, the Rapid Antigen test picks up active COVID-19 infection. Rather than antibodies to the disease.
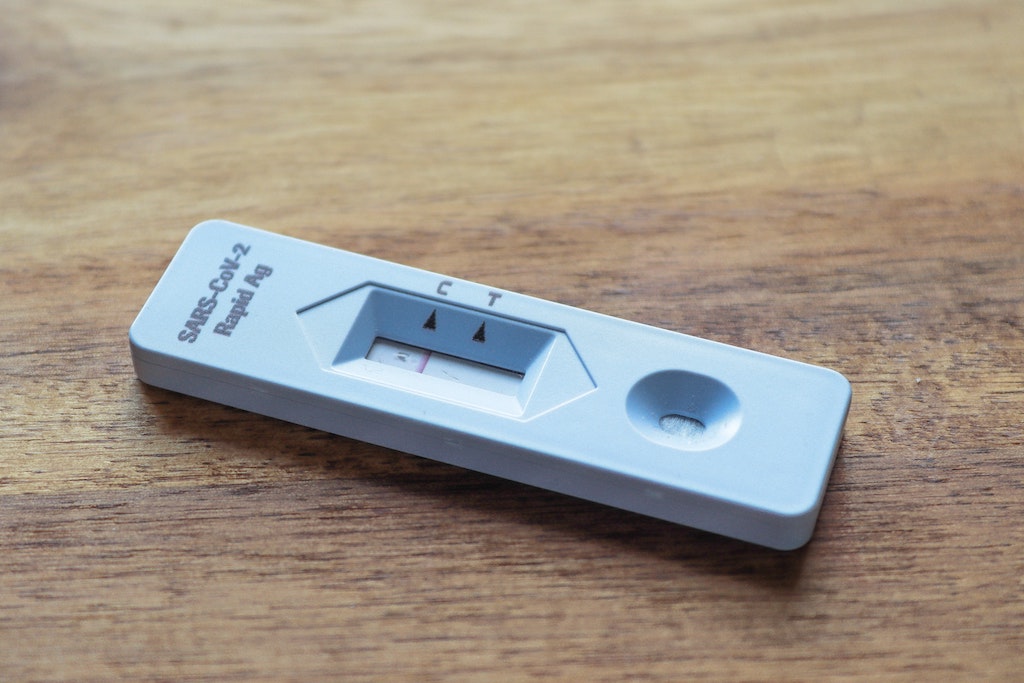
A nasopharyngeal sample is placed on a small absorbent pad. This is then drawn along the pad via a capillary line to a strip coated in antibodies. These antibodies bind to SARS-Cov-2 proteins.
If these proteins are present, this presence will show as a coloured line on the test. This indicates infection.
Rapid Antigen Test downsides
Since its first use the Rapid Antigen test has made incredible strides in accuracy.
As at March 2021, what the Rapid Antigen test gained in speed, it sacrificed in accuracy.
A review of 64 studies from Europe and the US showed a wide variance in accuracy between different brands of Rapid Antigen Test. The review also found that the tests were far better at identifying Covid-19 in people who had symptoms, than those who did not.
Sensitivity in symptomatic people ranged from 34% to 88%, with an average accuracy of 72%. In people without symptoms, rapid antigen testing correctly identified an average of 58% of those infected.
Since then the accuracy of Rapid Antigen tests has increased. Owing to improvements in the technology of the device itself and its operation.
In fact, in a more recent August 2021 study, researchers compared the validity of home antigen tests to PCR lab tests. The study collected results within days 0 to 12 of symptom onset. Home tests correctly identified 78.9 percent of people who did have the virus. And correctly identified 97.1 percent of people who didn’t have the virus.
This makes clear that rapid antigen tests rarely give a false positive result. A false positive is when you test positive for COVID-19 when you don’t actually have it.
Rapid Antigen Test - should you do it?
Considering the limited downsides just discussed, and that Rapid Antigen tests:
- provide results within minutes instead of days
- are more portable and accessible than lab tests
- are less expensive than lab tests
- do not need a specialist or lab
the answer is yes!
Rapid Antigen Tests are proving themselves in the early detection of Covid-19. And reducing the spread as a direct effect.
What about antibody testing?
Unlike the other two tests an antibody test does not tell you whether you're infected or not.
The immune systems generates antibodies after a week or two. After which time the virus should have been cleared from the system.
So antibody tests tell you who has been infected. And who should, as a result, be immune to the virus.